In the realm of mental health care, a one-size-fits-all approach to treatment often falls short. The complexity of the human brain, combined with the unique genetics, biology, and environmental history of each individual, means that what works for one person may be ineffective—or even harmful—for another. For decades, psychiatric medication management has relied on trial and error, with patients enduring weeks or months of side effects or minimal progress before landing on the right treatment plan. But now, a groundbreaking advancement in medical science is changing that narrative: pharmacogenomic testing.
Pharmacogenomics—the study of how a person’s genetic makeup affects their response to medications—is revolutionizing psychiatry. This cutting-edge approach to personalized medicine is helping clinicians make more informed decisions about prescribing psychiatric medications by identifying which treatments are likely to work best for each individual.
At Foundations Group Behavioral Health, we are proud to incorporate pharmacogenomic testing into our evidence-based mental health programs. This approach enhances our ability to provide effective, individualized care that supports lasting recovery and mental wellness.
What Is Pharmacogenomic Testing?
Pharmacogenomic testing involves analyzing a patient’s DNA to understand how their body metabolizes specific medications. It focuses on genetic variants that impact liver enzymes responsible for drug metabolism, as well as receptors and transporters that influence drug efficacy and side effects. In psychiatry, where medication classes such as antidepressants, antipsychotics, mood stabilizers, and anxiolytics vary widely in their effects, this data is invaluable.
For example, two individuals may be prescribed the same antidepressant, but while one experiences dramatic improvements, the other may suffer side effects or see no improvement at all. These differences often trace back to variations in genes such as CYP2D6 or CYP2C19—enzymes that help break down many commonly prescribed psychiatric drugs. Pharmacogenomic testing helps identify such variations in advance, reducing the need for trial-and-error prescribing.
The Impact on Psychiatric Medication Management
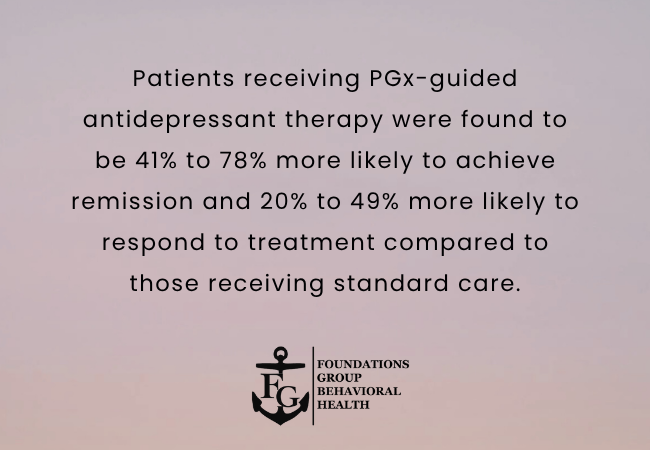
The goal of psychiatric medication management is to help individuals achieve emotional stability and symptom relief while minimizing side effects. With pharmacogenomic insights, providers can select medications that are more compatible with each person’s unique genetic profile, improving the likelihood of a successful treatment outcome.
At Foundations Group Behavioral Health, we incorporate pharmacogenomic testing into our Psychiatric Day Treatment Massachusetts services when clinically appropriate. This tool is especially helpful for clients who have experienced multiple medication failures or who suffer from complex psychiatric conditions requiring finely-tuned interventions.
The benefits of pharmacogenomic testing in psychiatry include:
- Faster therapeutic outcomes: Patients may find the right medication sooner, minimizing the distress caused by prolonged symptom instability.
- Reduced side effects: Knowing which medications a person is likely to tolerate can reduce the likelihood of adverse reactions.
- Increased medication adherence: Patients are more likely to stick with a treatment plan when it is effective and causes fewer unpleasant effects.
- Informed decision-making: Providers and clients can collaborate on treatment decisions with a clearer understanding of potential medication outcomes.
Who Can Benefit from Pharmacogenomic Testing?
Pharmacogenomic testing is especially beneficial for individuals who:
- Have not responded well to multiple psychiatric medications
- Have experienced severe side effects from common treatments
- Have a history of treatment-resistant depression, anxiety, bipolar disorder, or psychotic disorders
- Are beginning psychiatric treatment for the first time and want to minimize trial and error
This testing is also increasingly used in Outpatient Mental Health Therapy Massachusetts, where clients may be managing long-term medication plans while engaging in talk therapy, skills development, and community support.
Integrating Pharmacogenomics into Mental Health Treatment
At Foundations Group Behavioral Health, pharmacogenomic testing is used as part of a holistic, multidisciplinary approach. Genetic insights are combined with comprehensive clinical assessments that consider a person’s psychiatric history, trauma background, medical conditions, and psychosocial stressors.
We understand that no genetic test can replace the need for human insight and compassionate care. Medication is just one component of a broader mental health treatment plan. While pharmacogenomics can guide the choice of medication, it works best when paired with therapy, peer support, healthy lifestyle changes, and personalized goals for recovery.
This approach is particularly important in Mental Health Treatment Programs Massachusetts that serve individuals with complex diagnoses, co-occurring disorders, or trauma-related conditions. By integrating pharmacogenomics into these programs, we are better able to support our clients in achieving emotional balance and long-term stability.
Pharmacogenomics and Trauma-Informed Care
For individuals enrolled in our Trauma Disorder Treatment Program Massachusetts, pharmacogenomic testing adds another layer of personalization. Trauma can fundamentally alter brain chemistry, making medication response less predictable. Many trauma survivors are highly sensitive to side effects or may have developed mistrust around psychiatric treatment due to past experiences.
By providing clear, science-backed rationale for medication choices, pharmacogenomic testing helps build trust between client and clinician. It also enables a more informed, collaborative approach to care—empowering clients to take an active role in their recovery journey.
Addressing Misconceptions and Ethical Considerations
While pharmacogenomic testing holds tremendous promise, it is not without its limitations and misconceptions. It’s important to recognize that:
- The test does not diagnose mental health conditions.
- It cannot predict how effective a drug will be with absolute certainty.
- It should not be the sole factor in determining treatment.
Instead, pharmacogenomic testing should be seen as one more tool in a comprehensive psychiatric toolbox. Ethical considerations, including informed consent, data privacy, and the responsible interpretation of results, are also central to the way we implement genetic testing at Foundations Group Behavioral Health.
We ensure that all testing is conducted with transparency, and results are explained in a supportive, educational manner. Our clinicians guide clients through their results, helping them understand what their genetic profile means in the context of their treatment options.
Why Choose Foundations Group Behavioral Health?
As a trusted Behavioral Health Treatment Center Massachusetts, Foundations Group Behavioral Health is committed to delivering cutting-edge, compassionate mental health care. We recognize that medication is not a one-size-fits-all solution, and we take pride in offering progressive treatment options like pharmacogenomic testing to support our clients’ unique recovery paths. With an expert clinical team, trauma-informed care practices, and a focus on innovation, we empower our clients to take control of their mental wellness.
Conclusion
The future of psychiatry lies in personalized medicine—and pharmacogenomic testing is at the forefront of this evolution. By using genetic insights to inform psychiatric medication choices, clinicians can reduce the trial-and-error process, minimize side effects, and help individuals achieve better mental health outcomes more quickly.
At Foundations Group Behavioral Health, we believe that mental health treatment should be tailored to each individual’s needs, biology, and life experiences. If you or a loved one is navigating the challenges of mental illness and seeking a more effective path forward, we invite you to learn more about how personalized psychiatry can support your journey. Call us today at (833) 986-2594 to learn how we can help you take the next step toward healing.
Frequently Asked Questions (FAQs)
What is pharmacogenomic testing in psychiatry?
Pharmacogenomic testing analyzes a person’s DNA to determine how they may respond to psychiatric medications. This helps providers select medications that are more likely to be effective and cause fewer side effects based on the individual’s genetic makeup.
Who should consider pharmacogenomic testing?
This testing is particularly useful for individuals who have experienced multiple medication failures, have treatment-resistant conditions, or are starting psychiatric treatment and want to minimize the trial-and-error process.
Is pharmacogenomic testing accurate?
Pharmacogenomic testing offers valuable insights but is not 100% predictive. It should be used in combination with a thorough clinical assessment and ongoing therapeutic support to guide medication management effectively.
Does insurance cover pharmacogenomic testing?
Some insurance plans may cover pharmacogenomic testing when deemed medically necessary. It’s important to check with your insurance provider and discuss coverage options with your treatment center.
Is the testing process invasive or complicated?
Pharmacogenomic testing is usually simple and non-invasive. Most tests involve a cheek swab or saliva sample, which is then sent to a lab for analysis. Results typically return within a few days.








