You’ve been here before: therapy that gets close but never quite hits the mark, medications that help a little—but not in the ways you hoped. You may have thought, If I just tried harder, If I just waited longer, If I just found the right person, it would finally click. But when one issue gets treated in isolation—like anxiety without substance use, or depression without trauma history—the root often stays buried.
This is what dual diagnosis treatment in Massachusetts addresses. It’s not just a buzzword—it’s a game-changer for anyone caught in the cycle of care that never quite heals. At Foundations Group Behavioral Health in Massachusetts, we’ve seen how powerful an integrated approach can be for people who feel like treatment “didn’t work.” Because when you see and treat the whole picture—mental health and substance use together—progress stops looping and actually moves forward.
1. Dual Diagnosis Defined: More Than Co‑Occurring Conditions
A dual diagnosis, also known as a co‑occurring disorder, refers to the presence of both a mental health condition and a substance use disorder at the same time. These conditions don’t just appear together—they feed each other in ways that make single focus treatment often ineffective.
Common pairings include:
- Anxiety + Alcohol or Benzodiazepines: You manage anxiety by drinking—but end up with rebound effects and tolerance.
- Depression + Cannabis or Stimulants: You chase the high, but crash deeper, reinforcing hopelessness.
- PTSD + Opioids or Alcohol: You numb, but unresolved trauma resurfaces when substances fade.
- Bipolar disorder + Cocaine or meth: You self-medicate mood swings, exacerbating cycles of mania and despair.
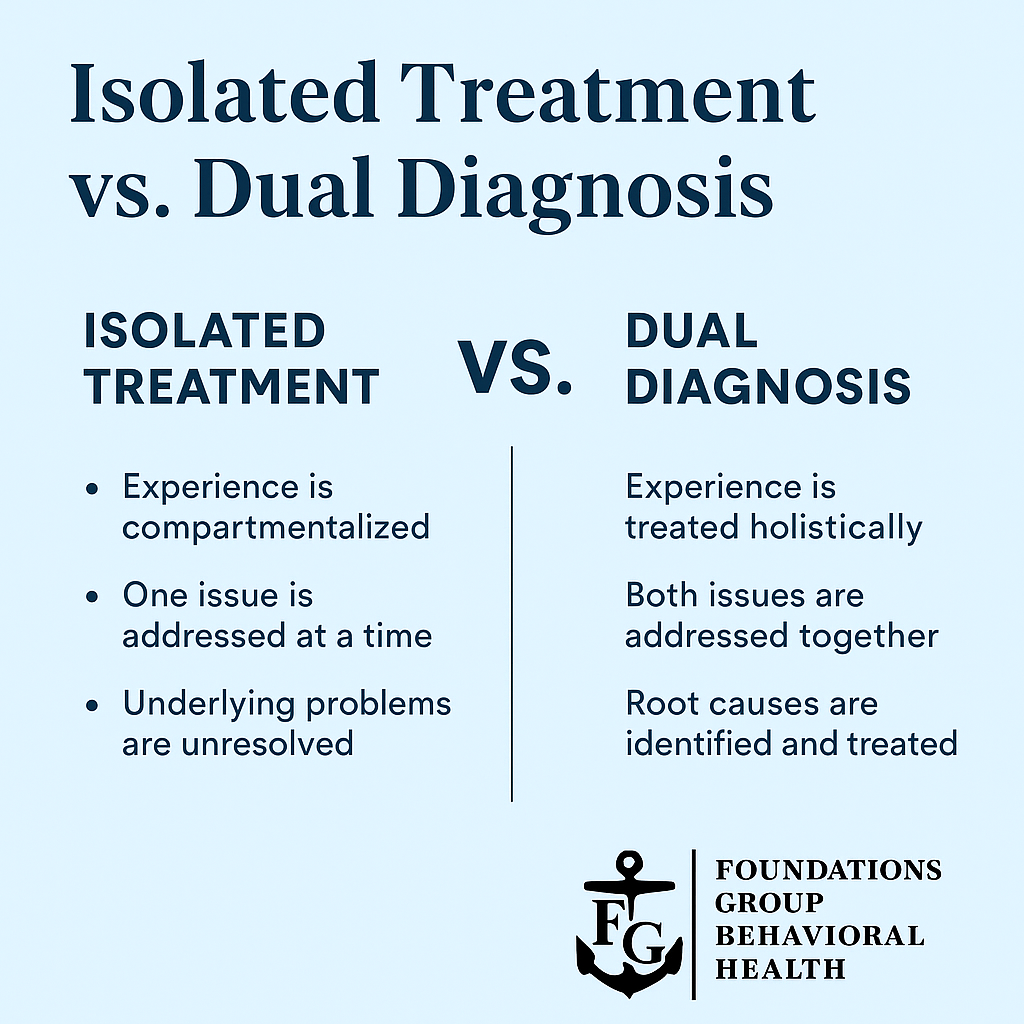
Dual diagnosis treatment means treating both conditions simultaneously, with a unified plan—because treating one in isolation often leads to symptom swapping, relapse, or burnout.
2. Why Standard Treatment Often Fails You
Here’s the reality: many treatment programs are siloed.
- A typical mental health clinic may ask, “Are you using drugs?” and then focus only on your anxiety or depression.
- A substance use rehab might dismiss trauma or mental health as secondary—”get clean first, and maybe then you’ll feel better.”
If you’ve been through both and felt like you’re just treading water, it’s not because you’re broken. It’s because the system is designed that way, and that stops real healing from happening.
Dual diagnosis care flips the script: your mental health and substance use are seen as interwoven—and deserving of integrated support.
3. What Makes Integrated Care Different
At Foundations Group, dual diagnosis care includes:
A) In-Depth Assessment
We use formal screenings for mental health and substance use, ensuring nothing is overlooked.
B) Medical and Psychiatric Support
If medications can stabilize mood, reduce cravings, or manage withdrawal, we’ll get that aligned—as part of your full treatment plan.
C) Therapy that Fits You
Treatment is tailored—whether it’s trauma-informed CBT, DBT, motivational interviewing, or relational approaches.
D) Substance‑Focused Support
You learn relapse prevention, triggers, cravings—within the same framework that addresses anxiety, depression, or trauma.
E) Group Therapy That Resonates
Our groups bring together people working through anxiety and recovery—so you’re not compartmentalizing your journey.
F) Holistic Life Skills
We teach you how to manage sleep, build community, balance responsibilities—so you can live beyond symptoms.
The result? A cohesive roadmap where your challenges and your healing are honored together.
4. How To Know If You Might Need Dual Diagnosis Care
You don’t have to be terrified to benefit from this approach—even if things are quietly unsteady.
Consider dual diagnosis treatment if:
A) You’ve tried other care but feel stuck.
No matter how many therapies or providers you’ve tried, something always remains unresolved.
B) You use substances to cope with emotions.
Even occasional use of alcohol, cannabis, or prescription meds to self-medicate hints at a deeper pattern.
C) Symptoms overlap and amplify.
Your mood, sleep, concentration, or relationships suffer only when you use—but stabilize when you don’t.
D) You’ve experienced relapse or flare-ups.
Backslides are common—but when your feelings and use cycle up together, a new level of care is needed.
E) You sense there’s more beneath the surface.
You may feel like you’re “not showing all of you” in therapy because substance use feels messy or shameful.
If any of these hit close, it might be time to work with a provider who can follow all the threads.
5. The Real Benefits of Dual Diagnosis Treatment
Trying dual diagnosis care was a turning point for many of us who felt treatments kept missing something.
What changes when you integrate your care?
🔹 Less relapse risk
When cravings, stressors, and emotional triggers are addressed together, it’s easier to maintain progress.
🔹 Faster breakthroughs
Patterns untangle faster when you don’t have to hide a part of your story from your provider.
🔹 More tailored strategies
Your coping plans aren’t generic—they’re based on your unique profile of anxiety, trauma, substance use, and healing style.
🔹Better quality of life
As symptoms ease and substance use declines, you reclaim focus, energy, and hope for what’s next.
When you’re treated as the whole person you are, you don’t just feel less stuck—you start feeling possible again.
Common Questions About Dual Diagnosis Treatment
Q: Can I be “too far gone” for integrated care?
A: No. Everyone benefits from seeing their full story. Dual diagnosis programs support people at all stages—early, advanced, or managing complex trauma.
Q: Isn’t this just therapy with a side of rehab?
A: It’s more than that. It’s seamless care that blends evidence-based practices across domains—without forcing a split approach.
Q: How long does treatment take?
A: Many clients start with a Partial Hospitalization or Intensive Outpatient program (4–6 weeks), then transition to supportive care. It’s all tailored to your pace and goals.
Q: What if I tried treatment before—and it didn’t work?
A: You’re not alone. But integrated care often is the missing piece. When your full experience is seen, healing starts to happen differently.
Q: Does insurance cover this?
A: Most insurance plans support dual diagnosis care—a combination of mental health and substance use services. Our team helps with benefits verification and coordination.
Ready to Get the Right Kind of Care?
If therapy alone hasn’t brought relief—or if treatment feels like it’s one step forward, two steps back—dual diagnosis treatment could finally shift things.
At Foundations Group Behavioral Health in Massachusetts, we offer integrated, evidence-based programs designed to treat your full, complex story—not fragments of it.
Call us at (888) 685-9730 or Contact Us.








