It’s a weird feeling: looking fine on paper, holding it together in front of others, but deep down…you know something’s off.
Maybe you’re not in crisis. Maybe you’re even “functioning.” But inside? There’s a dullness. A disconnect. A sense that your emotions are muted, your spark’s gone, or you’re operating on autopilot.
For people living with bipolar disorder, this is more common than most realize. And yet, many who experience this plateau feel guilty or ashamed for even considering going back to treatment. Like they’re admitting failure. Like needing more support means they’ve lost progress.
That’s a lie your illness wants you to believe.
Returning to bipolar disorder treatment in Cape Cod, MA isn’t going backward—it’s an act of insight, growth, and fierce self-respect.
Let’s talk about why.
You’re Not Starting Over. You’re Starting From Experience.
Coming back to treatment doesn’t mean you’re “back at square one.” Far from it.
The first time around, you may have been overwhelmed—barely surviving symptoms, clinging to structure, figuring out what bipolar disorder even was. Now? You’re not that person. You’ve done hard work. You’ve learned tools. You’ve seen what helps and what doesn’t.
So when things start to feel stuck or unmanageable again, stepping back into care isn’t retreat—it’s recognition.
You’re responding to what’s real. And that’s maturity, not regression.
Emotional Stuckness Is a Symptom—Not a Moral Failing
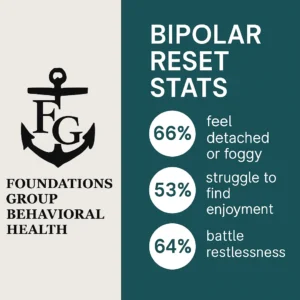
Let’s name it clearly: bipolar disorder doesn’t only show up in manic episodes or deep depression. Sometimes it shows up as:
- Emotional detachment
- Losing interest in relationships
- Unexplained irritability or restlessness
- Trouble sticking with routines
- Feeling like nothing matters
And when you’ve been stable for a while, these subtler symptoms can feel confusing. Maybe even shameful. You think: I should be doing better than this. Or worse: If I go back to treatment, what will people think?
Here’s the truth: needing renewed support is part of managing a chronic condition. You’d never shame a diabetic for adjusting their insulin. Why should mental health be different?
Flat Isn’t Fine—And “Not In Crisis” Isn’t the Goal
When you’ve lived with severe symptoms, your bar for what’s “fine” can get dangerously low. If you’re not suicidal, not manic, not melting down—it must be good enough…right?
But you deserve more than emotional survival. You deserve clarity. Joy. Connection. Feeling like yourself.
And if you’re feeling emotionally hollow, foggy, or checked-out? That’s not failure. That’s data. It’s your brain saying: Hey, something needs attention.
Bipolar Disorder Changes Over Time—So Should Your Treatment
One of the trickiest parts of managing bipolar disorder long-term is that your brain, body, and life circumstances don’t stay the same.
- Hormonal shifts
- Grief or major life changes
- Job stress
- Medication tolerance
- Isolation
Any of these can disrupt a previously effective treatment plan. That’s not because you did something wrong. It’s just reality.
And when reality changes, your care should too.
If you’ve been wondering whether your current plan still fits, or if you’ve outgrown what once worked—it might be time to revisit care with a fresh lens.
There’s No Prize for White-Knuckling
You don’t get a medal for toughing it out alone. There’s no trophy for waiting until things fall apart before asking for help.
You’ve already proven your strength. Now you get to prove something else: wisdom.
Re-engaging in care before things implode? That’s wisdom. That’s maturity. That’s what long-term bipolar disorder management actually looks like.
And you’re not the only one doing it.
At Foundations Group Behavioral Health, we regularly work with returning clients—people who’ve done the work, hit a plateau, and are ready to reconnect.
Whether it’s a short-term stabilization, medication re-evaluation, or a deeper dive into emotional processing, our bipolar disorder treatment program in Barnstable County, MA is here to support your next chapter—not rewrite your past.
You Deserve a Plan That Matches Who You Are Now
What helped you a year ago might not be what helps you now. And that’s okay.
Coming back to treatment gives you access to:
- New evidence-based strategies
- Updated medication insights
- A fresh therapeutic lens
- Group or individual therapy that speaks to where you’re currently at
- Community with others who understand long-term management
That last one is huge. Isolation is a known trigger for mood episodes—and it’s often a quiet one. Looking for bipolar disorder treatment in Falmouth, MA? Don’t underestimate the impact of being seen, known, and supported again.
What Returning to Treatment Actually Looks Like
Let’s demystify it.
Re-engaging doesn’t have to mean a full-time program or going “all the way back” to where you started. It might look like:
- A brief intensive outpatient tune-up
- Medication reassessment and support
- Short-term group therapy for mood regulation
- Reconnecting with a familiar therapist
- Exploring deeper emotional work that wasn’t possible earlier
It’s about targeted care—not repeating everything from scratch.
FAQ: Returning to Bipolar Disorder Treatment
Do I need to be in crisis to go back to treatment?
No. In fact, coming back before crisis hits is one of the smartest, strongest things you can do. Emotional numbness, low motivation, or persistent unease are valid reasons to seek support.
What if my friends or family think I’ve “relapsed”?
You don’t owe anyone a crisis to justify your care. Returning to treatment is not a sign of relapse—it’s a sign of self-awareness and commitment to your mental health.
How long will I need to stay in treatment?
That depends on what you’re seeking. Some people benefit from short-term support to recalibrate. Others choose to dive deeper into longer-standing issues. We’ll work with you to create a plan that fits your goals.
Will I be judged for coming back?
Absolutely not. Many of our clients return for additional support at different points in life. You’ll be met with respect, compassion, and clinical insight—not judgment.
What if I’m not sure what I need?
That’s okay. We’ll help you figure it out. Whether it’s an assessment, a consultation, or a space to explore what’s changed, you don’t have to walk in with answers.
You Can Reconnect Without Regret
The part of you that’s still checking in with this blog—that’s the part that wants more. Not more chaos. Not more drama. More connection. More clarity. More you.
You don’t have to stay emotionally numb. You don’t have to carry this alone. You’re allowed to want better—even when things don’t look “bad enough.”
Returning to bipolar disorder treatment isn’t a setback. It’s a next step.
And at Foundations Group Behavioral Health, we’re here when you’re ready to take it.
Ready to reconnect to care that fits the version of you today?
Call 888-685-9730 or visit our bipolar disorder treatment in Cape Cod, MA to learn more.