You made it to the coveted 90-day mark. You’ve sat in the therapy chairs, completed the program, earned the milestone chips. Then—somewhere after the emails, the resumes, the job stress—you realized: you’re back where you started.
If you’ve relapsed, and are telling yourself “I’ve just got depression,” pause for a moment. That answer is incomplete. It might feel safer to believe your issue is one-dimensional—but what if that narrative is the very thing keeping you stuck?
At Foundations Group Behavioral Health in Massachusetts, we’ve seen time and again that relapse often isn’t about weakness or failure—it’s a signal. One sign that therapy treated symptoms, not root causes. That is where dual diagnosis treatment comes in. It’s not just treatment—it’s honesty.
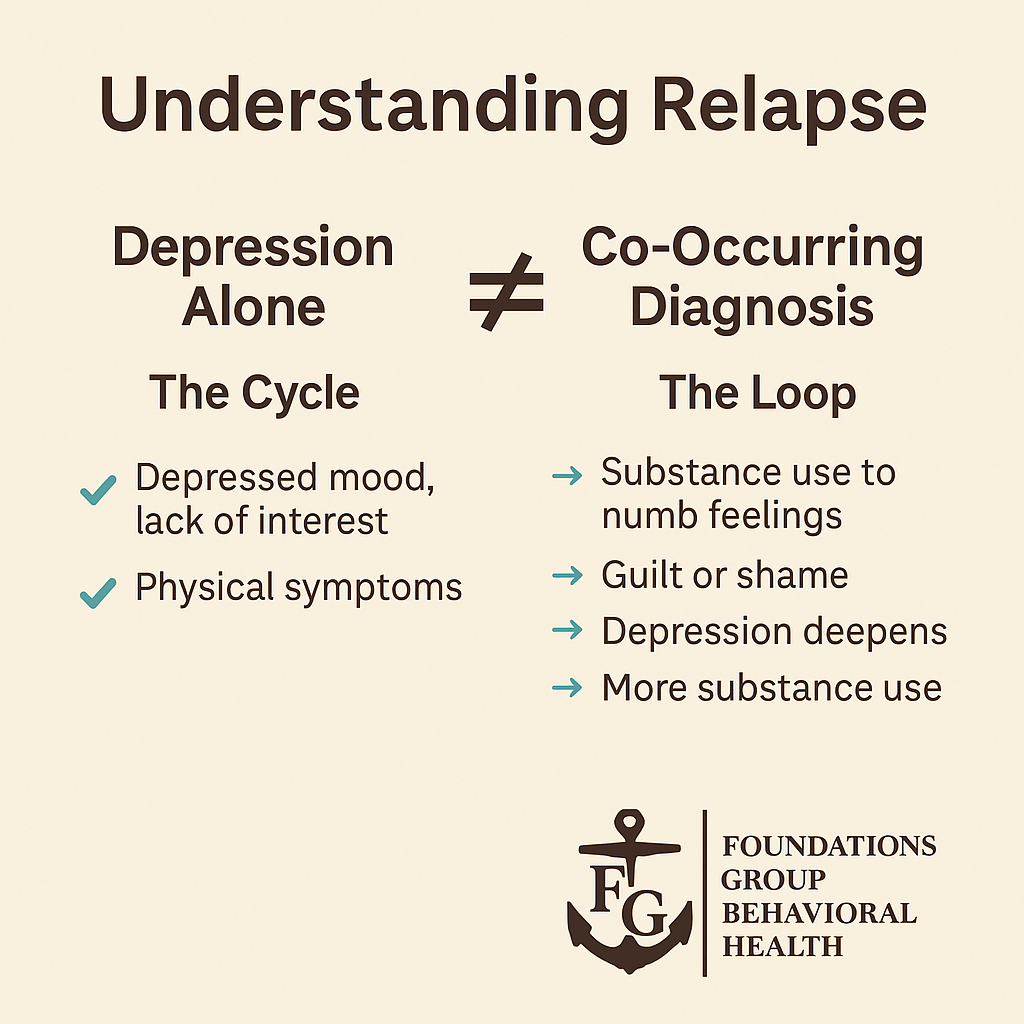
1. The Difference Between Depression Alone and a Co-Occurring Diagnosis
Depression can drain you. It clouds your mood, crushes motivation, and makes everything feel heavy. Yet it’s not always the only player in the room.
In dual diagnosis, there are two—mental health and substance use—entangled in ways that feed each other. Using alcohol to numb sadness leads to guilt, which deepens depression, prompting more use. It becomes a loop of mutual reinforcement.
When both conditions exist together, treating only one is like applying a band-aid to a wound that needs stitches.
2. Why Focusing Solely on Mood Doesn’t Prevent Relapse
Therapy for depression offers essential insights: tracking mood, reframing thoughts, building routines. But without targeted support for substance use—like understanding triggers, managing cravings, and relapse prevention—making progress is like walking with one shoe off.
Many alumni relapse not because they gave up on recovery, but because treatment wasn’t tailored to the whole complexity of their situation. Once life pressure returns, the substance-use strategies remained underdeveloped.
3. Dual Diagnosis Treatment: Building Full-Spectrum Resilience
A dual diagnosis approach integrates mental health and addiction care through:
- Comprehensive assessment – examining mood, substance use, trauma
- Medication management – addressing both depression and withdrawal
- Integrated therapy – think CBT, DBT, trauma-informed rehab
- Addiction-specific tools – relapse prevention, craving interruption
- Peer-based support – with others who juggle both sides
- Life skills training – building balance in work, stress, relationships
You no longer have to choose one part of the story. Instead, you create a holistic plan that follows you across environments, triggers, and milestones.
4. Why Relapse Doesn’t Mean Failure When You Embrace Integration
Relapse isn’t an accident or a lack of willpower—it’s often a sign that a layer of challenge wasn’t fully addressed. In integrated care, relapse is data—not ethics.
Your team looks beneath the lapse: Was it emotional pain? Relationships? Job stress? Trauma? And then they reconfigure your plan with new clarity and compassion.
That structure reassures your burnout isn’t a personal shortcoming—it’s a cue to pivot and expand your support.
5. How to Move Forward If You’ve Just Sobered Up Again
If you relapsed and are wondering, “Do I start over…or double down?”, here’s a guide:
- Own the insight – Not “I failed,” but “I learned something.”
- Assess all domains – Mood, cravings, daily habits, triggers.
- Look for integrative care – Is the program offering us both mood and addiction tools?
- Check the support team – Do they specialize in dual diagnosis? Are they trained across disciplines?
- Give yourself credit for trying again – Relapse doesn’t wipe out what you’ve built.
Dual diagnosis care doesn’t discard what you did right—it builds on it. It recognizes your effort and adds the missing pieces.
FAQs: Honest Answers for the Relapsed Alumni
Q: I’ve already been through treatment—do I really need to do it again?
A: Not from scratch. You’ve done important work. With dual diagnosis care, we re-engage with your history, pick up where treatment left off, and adapt to your current life stage.
Q: I thought depression was the problem—but every time I felt better, I drank again.
A: That disconnect is common. When one condition is treated in isolation, the unaddressed one tends to push back. Dual diagnosis treatment helps both stabilize together.
Q: Do I have to admit addiction to enter this program?
A: You only need to tell the truth. If substance use is causing pain or impacting your goals, we can support you—even if you’re unsure what to call it.
Q: Will they do group therapy? What if I don’t fit in?
A: Yes—but our groups are co-occurring focused, so everyone is navigating both emotional and substance challenges. You’re not the only one balancing both worlds.
Q: Does insurance cover this?
A: Most insurance plans allow billing for joint mental health and addiction services. We’ll help you verify your benefits—so you’re not left wondering.
Start Again. Smarter. Stronger.
After 90 days, relapse doesn’t signal failure—it signals that you need a broader treatment map. You need his toolset expanded, not erased.
If you’re tired of repeating old cycles—and ready to build from what you have—dual diagnosis treatment offers the honesty and structure you need.
At Foundations Group Behavioral Health in Massachusetts, we see your effort, respect your courage, and offer the integrated care that actually works.
Call (888) 685-9730 or Contact Us.








