Your 20-year-old is using again.
You saw the signs. You smelled it. You felt it in your gut before you had proof. Maybe it’s weed. Maybe something stronger. Maybe it’s a mix of everything, cycling faster than you can keep track. But the scariest part isn’t the substance—it’s the mood underneath it.
The energy that burns too bright, too fast.
The rage you don’t recognize.
The depressive crashes that keep them in bed for days.
You’ve probably asked yourself more than once:
Is this bipolar disorder?
And maybe even more painfully:
What if they’re using because they know it too—and they’re scared?
At Foundations Group Behavioral Health in Cape Cod, MA, we work with parents who are holding all of this: the fear, the confusion, the love, and the helplessness. You’re not failing. You’re just up against something that’s incredibly complex—and often misunderstood.
This blog is here to clarify what bipolar disorder treatment really requires—and why substance use must be treated at the same time.
Because the truth is: treating one without the other just doesn’t work.
Mood Disorders and Substance Use Don’t Just Co-Exist—They Interact
Let’s start with the big picture:
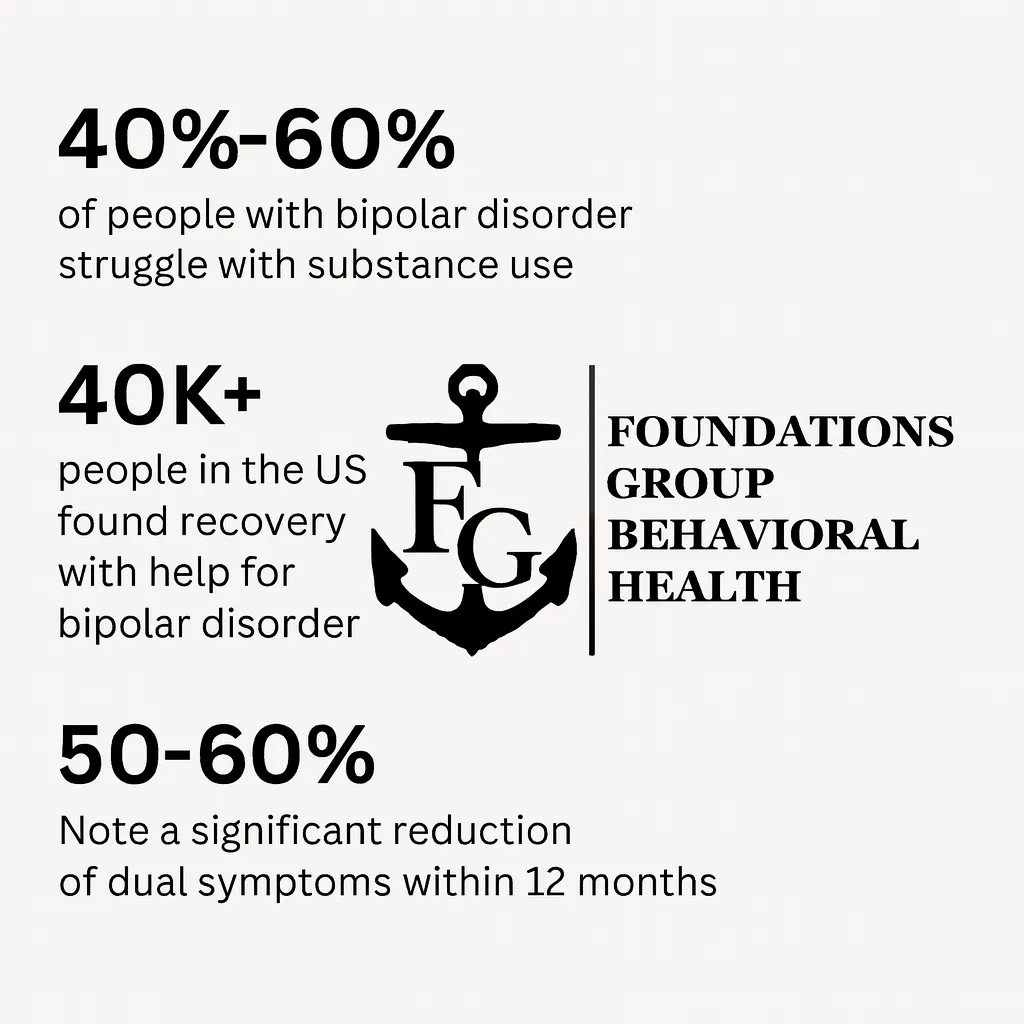
It’s estimated that 40–60% of people with bipolar disorder also struggle with substance use.
Why? Because when your brain oscillates between depression and mania, substances become emotional shock absorbers:
- Cannabis to slow the racing thoughts
- Alcohol to turn down the volume of rage or grief
- Stimulants to escape the paralysis of depression
- Benzos to quiet the anxiety between episodes
What starts as self-medication often becomes dependency—and what looks like a “drug problem” is often the tip of the iceberg.
If your child has a diagnosis—or even just the symptoms—of bipolar disorder, and they’re using substances, you cannot separate the two.
Treatment has to look at both. Together. Always.
The Risk of Ignoring Substance Use? A Loop You’ve Already Lived
Maybe this sounds familiar:
- Things are okay—for a minute.
- They stop taking meds, or never start.
- They get manic or deeply depressed.
- They use something to manage it (weed, alcohol, etc).
- They spiral. You intervene.
- They stabilize just long enough to convince everyone they’re fine.
- Repeat.
You’ve seen the loop. You’ve felt the heartbreak of a week that felt better—until it wasn’t. You’ve clung to the hope that this time would be different, only to be blindsided again.
This is not because they don’t want to get better. It’s because they’re not getting the kind of care that actually works.
And here’s the hard truth:
Stabilizing bipolar symptoms without addressing substance use is like putting out a fire while someone’s still pouring gasoline.
What Real Bipolar Disorder Treatment Looks Like
It’s not just meds. It’s not just therapy. And it’s definitely not just hoping they’ll figure it out on their own.
At Foundations Group Behavioral Health, bipolar disorder treatment includes:
- Psychiatric care, with a provider who understands the subtle shifts of bipolar disorder and how substances mimic or mask symptoms.
- Dual diagnosis therapy, meaning we treat both the mood disorder and the substance use with equal seriousness.
- Trauma-informed care, because many of these young adults are carrying deeper wounds.
- Psychoeducation, so your child actually understands what’s happening in their brain and body.
- Family involvement, because you deserve clarity too—and boundaries can’t be built without context.
We’ve seen this work in Barnstable County and Falmouth, not just for the young adults in care—but for the parents who come to us burnt out, heartbroken, and scared.
Medication Helps, But It’s Not a Magic Fix
Let’s be honest—meds help. They can stabilize mood, prevent relapse, and create breathing room. But they aren’t a cure, and they don’t teach your child how to live with their mind. They don’t address the reasons your kid reaches for substances in the first place.
Without therapy, without skills, without a space to feel all the big feelings underneath the behavior, meds are just a leash. And for many young adults? That feels suffocating.
Real bipolar treatment builds something better:
Trust, insight, and ownership.
That’s when change sticks.
You Can’t Force Readiness, But You Can Invite It
A lot of parents wait until their child hits rock bottom. But with bipolar disorder, the bottom can come fast—and hard. A single manic episode can mean arrest, hospitalization, or worse.
You don’t have to wait for crisis. You can begin treatment conversations now.
We work with families at all stages of readiness, including:
- Parents whose children are still denying there’s a problem
- Young adults who say they’re “fine” but are clearly unraveling
- Families who’ve done 2-3 rounds of treatment and feel like nothing stuck
Your kid doesn’t need to be 100% ready. They just need one moment of openness. And you need support, so you don’t have to carry the entire weight of their future alone.
What Parents Can Expect in Dual Diagnosis Care
When your child enters a bipolar disorder treatment program that addresses substance use too, here’s what you can expect:
- A whole-person intake process, not just a checklist
- Flexible care levels (including outpatient and intensive options)
- Support for medication initiation or re-initiation
- Access to family sessions, focused on communication, boundaries, and education
- Ongoing updates and treatment planning with your involvement
If you’ve ever been left out of your child’s care—or made to feel like the problem—this is different. At Foundations, we believe parents are part of the healing process. Not obstacles to it.
FAQ: Bipolar Disorder, Substance Use, and What Comes Next
What if my child won’t stop using weed but takes their meds?
This is incredibly common. Cannabis is often seen as “less serious”—but it interferes with meds and worsens mood cycling. We explore the why behind use without shaming, and build buy-in for change over time.
What’s the difference between bipolar disorder and substance-induced mood swings?
Good question. It’s not always clear at first. Our assessment process helps differentiate, and we treat both possibilities while clarifying the true diagnosis.
They’ve been to treatment before and it didn’t work. Why try again?
Most programs treat either the mood or the substance—not both. When care is integrated, outcomes improve dramatically. Many of our clients have failed elsewhere and found stability here.
Will they need to stay in treatment long-term?
Not necessarily. Some need 2–3 months of structured care. Others need longer-term support. Our goal is to stabilize, empower, and transition to community-based support—not trap them in a system.
Can I get help even if my child refuses treatment?
Yes. We offer parent sessions, support groups, and guidance—even when your child won’t engage. Your healing matters too.
This Isn’t Just About Getting Them Back—It’s About Moving Forward Together
You miss them.
The version of them that laughed easily. That texted back. That wasn’t unpredictable, cruel, or unreachable. The child who loved playing guitar. Or painting. Or talking philosophy late at night.
You don’t want the past.
You want them. Whole. Clear. Free from whatever has its grip on them.
And that’s what real bipolar disorder treatment offers—when it addresses everything that’s going on, not just the diagnosis on the chart.
Call 888-685-9730 or visit our bipolar disorder treatment program in Cape Cod, MA to speak with someone who gets it.
You don’t have to wait for another crisis. You can start something different—today.