Complex trauma and dissociative disorders present some of the most significant challenges in mental health treatment. Unlike single-incident trauma responses, complex trauma results from prolonged and repeated exposure to harmful experiences—often beginning in early childhood. These can include neglect, abuse, or other violations of safety and trust. For individuals coping with the psychological imprint of such events, traditional therapy often falls short. Instead, specialized, adaptable outpatient approaches are necessary to help them recover in ways that honor their pace and their unique inner experiences.
Outpatient therapy—when thoughtfully designed—can become a stabilizing and transformative part of recovery for those facing these long-term effects. But it demands an understanding of trauma’s multifaceted impacts, a flexible therapeutic alliance, and tools that reach beyond basic talk therapy. Treating dissociative symptoms, emotional dysregulation, and attachment wounds takes time, consistency, and a great deal of sensitivity. Adapting outpatient therapy to meet these needs isn’t just a clinical preference—it’s an ethical imperative.
Understanding the Complexity of Trauma and Dissociation
Complex trauma occurs when harmful experiences—such as emotional neglect, physical abuse, or abandonment—take place over an extended period, particularly in formative years. Rather than producing the classic symptoms associated with post-traumatic stress disorder (PTSD), complex trauma often leads to pervasive difficulties in emotion regulation, identity formation, and interpersonal relationships.
Dissociation, often seen in individuals with a history of complex trauma, is the brain’s way of surviving what feels emotionally or physically inescapable. It may range from a sense of emotional numbness or zoning out, to identity fragmentation and memory loss. These symptoms are protective but can become deeply disruptive, especially when misunderstood or minimized in therapy settings.
Outpatient therapy that does not account for these factors risks retraumatizing individuals or encouraging premature processing of traumatic memories. An adaptive approach focuses instead on safety, pacing, and connection.
Creating Safety in the Therapeutic Relationship
The foundation of all effective trauma therapy lies in establishing a safe therapeutic relationship. For those with complex trauma, even this foundational task can take significant time and effort. A person who has learned through experience that closeness leads to harm will not instinctively trust even a well-meaning therapist. Safety, in this context, means emotional predictability, a nonjudgmental stance, and the therapist’s ability to tolerate a range of intense emotions without reacting.
Sessions must be paced in accordance with the client’s readiness. While goal-setting can be useful, rigid outcomes or timelines can mirror early dynamics of control and create barriers to engagement. The focus must remain on helping clients stay within a tolerable emotional window, rather than pushing for insight or resolution too quickly.
Therapists also must be trained to notice dissociative symptoms early. Clients may not recognize or report these experiences themselves. Instead, they may describe feeling “foggy,” “gone,” or “not real.” Skillful intervention involves grounding techniques, parts work (if appropriate), and an awareness of how certain therapeutic conversations can trigger internal shutdowns.
Structuring Sessions for Flexibility and Stability
Therapy for complex trauma should be structured—but not rigid. While some predictability fosters safety, clients with trauma histories often benefit from knowing that their internal experiences will be respected and not forced into a narrow framework.
This includes the therapist’s flexibility in how sessions unfold. Sometimes, a client may need to focus a full session on stabilizing from a flashback, rather than exploring its source. Other times, sessions might focus on somatic awareness, resourcing strategies, or navigating present-day triggers. What’s important is that the client feels in control of the process and trusts that therapy is a place for collaboration, not coercion.
It’s also important for clinicians to remember that trauma processing is not always verbal. Many individuals carry trauma in their bodies and may benefit from integrating practices like grounding techniques, breathing exercises, or gentle movement. Nonverbal therapies, such as art or music, can also help unlock emotions that feel too dangerous to articulate.
Working with Fragmentation and Parts
One of the more complex aspects of dissociative disorders is the presence of identity fragmentation—what some describe as “parts.” These internal parts can hold different memories, emotions, and even perspectives on therapy itself. Rather than seeing this as pathological, adaptive therapy recognizes that these parts have developed to manage trauma and protect the individual.
Therapists trained in models like Internal Family Systems (IFS) or Ego-State Therapy can help clients build communication and cooperation between parts without rushing toward integration. Outpatient therapy allows time for this process to unfold organically. It also encourages clients to notice patterns of dissociation or emotional withdrawal without shame or fear of rejection.
Crucially, the therapist must offer a stable presence even when different parts of the client present conflicting emotions or behaviors. It’s not uncommon for a client to trust their therapist deeply one week, and then enter a session with suspicion or hostility the next. Adaptive therapy sees this as part of the healing, not resistance.
Skill Building and Self-Regulation
For individuals healing from complex trauma, emotion regulation skills are essential. These include identifying emotions, developing distress tolerance, managing intrusive thoughts, and learning how to return to a state of calm after activation. Outpatient Mental Health Therapy Massachusetts provides a structured yet flexible setting where clients can learn and reinforce these skills over time.
While some clients may benefit from structured approaches like Dialectical Behavior Therapy (DBT), these skills should always be introduced with trauma sensitivity. If a client is feeling overwhelmed or shamed for struggling with a skill, therapy can quickly become unsafe. The goal is to empower clients with tools they can use between sessions, not to burden them with additional expectations.
Therapists may also integrate mindfulness practices, journaling prompts, or creative expression to support self-reflection and emotional containment. These approaches work especially well in outpatient care, where clients have the opportunity to apply skills in real-life situations between sessions.
Navigating the Role of Diagnosis and Treatment Planning
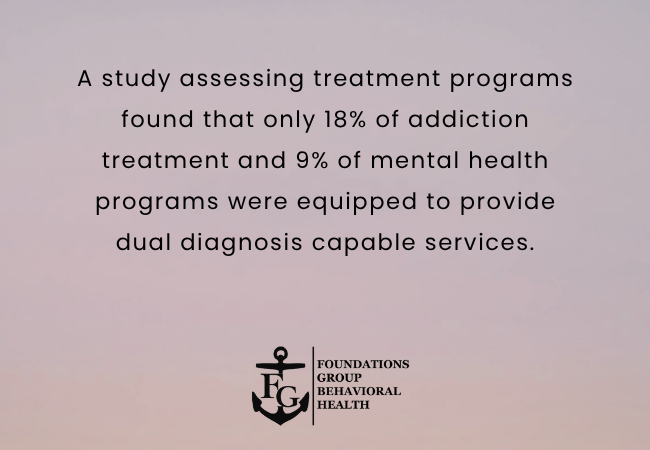
Clients with complex trauma and dissociative symptoms are often misdiagnosed with mood disorders or personality disorders before receiving accurate evaluations. A correct diagnosis—when delivered with compassion—can help reduce confusion and validate internal experiences. Still, labeling must never replace listening. Outpatient providers must recognize that symptoms like mood swings, self-harm, or substance use often arise from deeper, trauma-based origins.
Treatment planning should be collaborative and updated regularly. What works in one phase of healing may become counterproductive later. Because dissociative symptoms can fluctuate, clients benefit from plans that include grounding routines, backup support strategies, and a clear understanding of when to seek additional care if needed.
In some cases, longer-term or more intensive programs may be necessary. Programs such as a Trauma Disorder Treatment Program Massachusetts can provide higher levels of support when outpatient therapy alone is not sufficient. The key is for therapists and clients to work together in making those transitions with care, not crisis.
The Role of Community and Support Systems
Healing from complex trauma is not only about internal work—it also involves finding safe community. While outpatient therapy builds one consistent relationship, individuals may also benefit from peer groups, trauma-informed support groups, or activities that reconnect them with their creative or spiritual selves.
Families and partners, when included in therapy appropriately, can also become allies in the healing process. That said, boundaries and consent are essential—especially when relational trauma came from within the family system. A qualified outpatient therapist will guide this process with caution and respect for the client’s comfort level.
Why Choose Foundations Group Behavioral Health?
At Foundations Group Behavioral Health, we understand that trauma recovery is non-linear and deeply personal. As a trusted provider of Mental Health Therapy Massachusetts, we create customized outpatient therapy plans that address not only symptoms but the story beneath them. Our clinicians bring advanced training in trauma treatment, dissociation, and emotion regulation—and above all, we offer a space of respect, collaboration, and safety.
Conclusion
Recovering from complex trauma and dissociative disorders takes time, support, and the right therapeutic approach. With adaptive outpatient therapy that emphasizes safety, flexibility, and deep listening, individuals can begin to heal and build a more grounded, empowered sense of self. If you or a loved one is seeking compassionate trauma-informed care, Foundations Group Behavioral Health is here to help. Contact our Behavioral Health Treatment Center Massachusetts to learn more or schedule an appointment.
Frequently Asked Questions (FAQs)
What is outpatient therapy for complex trauma?
Outpatient therapy for complex trauma provides structured support while allowing individuals to live at home. It focuses on developing coping skills, processing traumatic experiences, and building emotional regulation without requiring residential care.
How is outpatient therapy different from inpatient care?
Outpatient therapy allows clients to attend scheduled sessions while maintaining daily responsibilities like work or school. In contrast, inpatient care involves full-time treatment in a residential setting. Outpatient therapy is ideal for those who need flexibility but still benefit from professional support.
Can outpatient therapy help with dissociative disorders?
Yes. Outpatient therapy is often adapted to treat dissociative disorders by focusing on grounding techniques, building a sense of safety, and addressing fragmented memory or identity concerns in a safe, consistent environment.
What types of therapy are used for trauma in outpatient care?
Common modalities include cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), EMDR (Eye Movement Desensitization and Reprocessing), and somatic therapies. These are tailored to the individual’s trauma history and symptoms.
How long does outpatient trauma therapy last?
The duration of outpatient trauma therapy varies by individual needs, ranging from several months to a year or more. Progress depends on the complexity of the trauma, goals of therapy, and consistency of attendance.