Something shifts.
Your child isn’t just overwhelmed anymore. They’re unreachable. Irritated by everything. Sleeping through life — or not sleeping at all. Maybe they’ve started saying things that make your chest tighten: “It doesn’t matter.” “I’m just tired.” “You’d be better off without me.”
If you’re here, you already know this isn’t typical sadness. It’s something heavier. And it may be time to consider real, structured support like a depression treatment program.
This is not an overreaction. It’s a parent paying attention.
Depression in Young Adults Can Escalate Fast
Severe depression doesn’t always announce itself dramatically. Sometimes it creeps. Other times it crashes.
What makes it especially frightening for parents is how quickly functioning can unravel.
A young adult who was managing school or work just months ago may suddenly:
- Withdraw from friends completely
- Stop responding to messages
- Drop classes mid-semester
- Quit a job without a backup plan
- Stay in bed 14+ hours a day
- Explode in anger over small requests
- Appear emotionally flat or detached
You may feel like you’re watching someone slowly disappear.
Depression at this level is not a bad mood. It’s not laziness. It’s not a character flaw.
It’s an illness that affects cognition, energy, perception, and motivation all at once.
And when it becomes severe, it can become dangerous.
Crisis Doesn’t Always Look Like Chaos
Many parents wait for a dramatic event to label something a crisis.
An ambulance. A hospitalization. A suicide attempt.
But crisis is often quiet.
It can look like:
- Talking about feeling like a burden
- Giving away personal items
- Saying life feels pointless
- Expressing guilt that feels extreme or distorted
- Indifference toward future plans
- Risky or reckless behavior
Severe depression narrows perspective. It creates tunnel vision where the future disappears.
Your child may not be actively planning to hurt themselves — but they may also not care if something happens.
That emotional numbness is serious.
And it deserves structured intervention, not just reassurance.
You Cannot “Love” Severe Depression Away
This is the part that hurts.
You can be deeply involved.
You can check on them daily.
You can sit beside them for hours.
And it still may not be enough.
Depression alters brain chemistry. It disrupts sleep-wake cycles. It distorts thinking. It changes appetite. It magnifies shame and minimizes hope.
It tells your child lies — in their own voice.
As a parent, you can offer support. But you cannot provide:
- Daily clinical monitoring
- Professional risk assessment
- Medication management when appropriate
- Structured therapeutic interventions
- Peer accountability
When depression becomes severe, home often becomes the place where symptoms worsen — not because you’re failing, but because unstructured time allows the illness to expand.
Love is powerful.
But love is not a treatment plan.
Why Structured Care Changes Outcomes
Structure is not about control.
It’s about containment.
Severe depression thrives in isolation and unpredictability. Days blur together. Sleep flips upside down. Motivation vanishes. Thoughts spiral unchecked.
Structured treatment interrupts that spiral.
In a formal depression treatment program, young adults step into:
- Consistent daily schedules
- Individual therapy
- Group therapy
- Psychiatric oversight
- Skills training
- Peer connection
- Ongoing safety monitoring
Structure creates external scaffolding while the internal framework is rebuilding.
Instead of lying in bed negotiating with intrusive thoughts, your child has somewhere to be. People expecting them. Clinicians assessing risk in real time.
Depression feeds on emptiness.
Structure fills space with support.
“What If They Refuse Help?”
This is one of the most painful realities parents face.
Young adults in deep depression often say:
- “Nothing will help.”
- “I don’t need that.”
- “I’m fine.”
- “It won’t work anyway.”
Hopelessness is a symptom — not a decision.
What we’ve seen repeatedly is that when treatment is presented calmly, clearly, and consistently, many young adults agree to try structured daytime care or multi-day weekly treatment.
Not because they suddenly feel optimistic.
But because they’re exhausted.
Sometimes the turning point isn’t hope. It’s fatigue from suffering.
You don’t have to win an argument. You just have to keep the door open.
The Cost of Waiting
Parents often hesitate because they don’t want to “overreact.”
But here’s the hard truth:
When depression reaches a severe stage, it rarely resolves on its own without intervention.
Waiting can mean:
- Academic withdrawal
- Job loss
- Social isolation
- Worsening suicidal ideation
- Substance use emerging as self-medication
- Longer recovery timelines
Early structured intervention often shortens suffering.
Depression untreated tends to entrench. Depression treated tends to stabilize.
That doesn’t mean instant happiness.
It means reduced risk. Improved function. Gradual return of clarity.
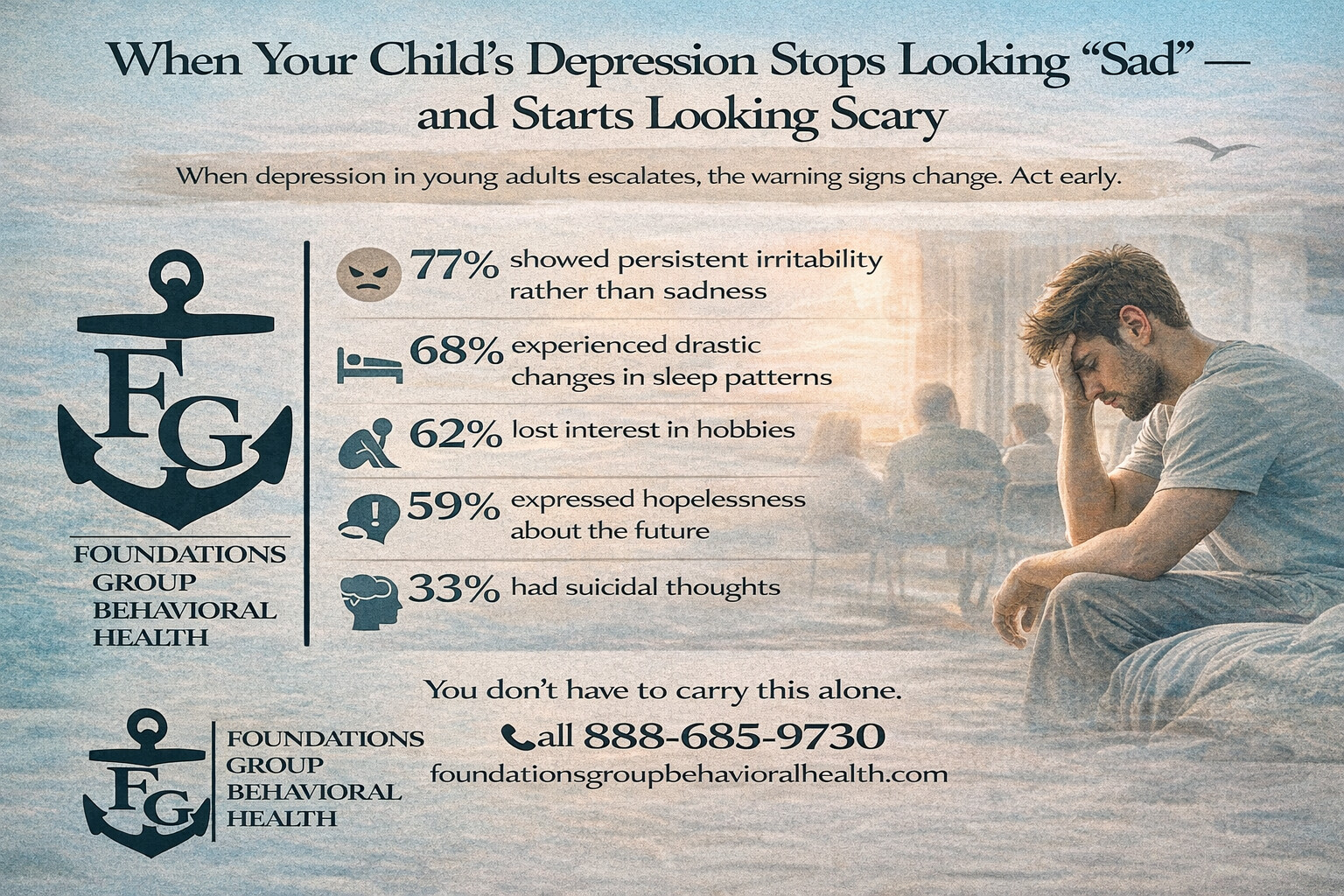
What Parents Often Notice First
Before young adults admit they’re struggling, parents frequently observe:
- Increased irritability instead of sadness
- Drastic changes in sleep patterns
- Loss of interest in hobbies
- Avoidance of responsibilities
- Emotional numbness
- Statements that reflect hopelessness
Depression doesn’t always cry.
Sometimes it goes silent.
Sometimes it lashes out.
Sometimes it just stops caring.
If your intuition is telling you something is very wrong — trust it.
FAQ: What Parents Need to Know About Severe Depression
How do I know if this is severe depression or just a rough phase?
A rough phase typically fluctuates. Severe depression persists and impairs daily functioning.
If your child is unable to maintain school, work, relationships, hygiene, or basic routines — and this lasts weeks or months — it’s more than a phase. When hopelessness or suicidal thoughts are present, it requires immediate professional evaluation.
Does structured treatment mean hospitalization?
Not necessarily. Many young adults benefit from structured daytime care or multi-day weekly treatment without requiring inpatient hospitalization.
Hospitalization is typically reserved for imminent safety risks. Other levels of care provide intensive support while allowing some independence. The right level depends on risk, stability, and clinical assessment.
Will medication automatically be required?
Not always. Medication decisions are individualized and based on psychiatric evaluation. Some young adults benefit significantly. Others focus primarily on therapy-based interventions. A structured setting allows careful monitoring rather than rushed decisions.
How long does structured treatment last?
Length varies based on severity, response to care, and individual needs.
Some young adults stabilize within weeks. Others require longer periods of structured support.
The goal is not to keep someone in treatment indefinitely — it’s to restore stability and build sustainable coping systems.
What if my child is over 18 and refuses consent?
Once someone is legally an adult, parents cannot force voluntary treatment unless safety thresholds are met for involuntary evaluation.
However, you can:
- Set boundaries at home
- Offer clear options
- Encourage evaluation
- Seek guidance from professionals
- Participate in family support sessions
You are not powerless — even when it feels that way.
Can severe depression fully improve?
Yes. With appropriate support, young adults can and do recover from severe depressive episodes.
Recovery may not look like instant joy. It looks like:
- Improved sleep
- Reduced suicidal thinking
- Increased motivation
- Return of future-oriented thinking
- Re-engagement with life
Depression tells your child nothing will change.
Structured support quietly proves that wrong.
You Don’t Have to Carry This Alone
If you’re reading this at 2 a.m., searching phrases you never thought you’d Google, we want you to hear this clearly:
You are not dramatic. You are not failing. And you are not alone in this.
Severe depression is frightening — especially when it’s your child.
The earlier you seek structured support, the more options you have.
Call 888-685-9730 or visit our Depression treatment program services in to learn more about our Depression treatment program services in Falmouth, MA.
Sometimes the bravest thing a parent does is say, “This needs more help than I can give.” And that is not weakness. That is love.